Medicalese
 80 yo WF c PMH NIDDM x10yrs, HTN, c/o HA. Ø N/V/CP/SOB/Abd pain. PE: AAOx3, NAD, PERRLA, EOMI, MMM, Ø JVD, S1 S2, HRRR, LCTA, Abd NT/ND, BPPP. VS: 98.3° 150/80 80 18…
80 yo WF c PMH NIDDM x10yrs, HTN, c/o HA. Ø N/V/CP/SOB/Abd pain. PE: AAOx3, NAD, PERRLA, EOMI, MMM, Ø JVD, S1 S2, HRRR, LCTA, Abd NT/ND, BPPP. VS: 98.3° 150/80 80 18…
About three years ago, I wrote a post titled “Second Language” in which I talked about how learning medicine comes with learning an entirely new set of vocabulary, like a second language. Now, after 11 months of seeing patients, writing progress notes, H&P’s, and consult notes, I’ve picked up another language that builds upon the language of medicine: medical abbreviations.
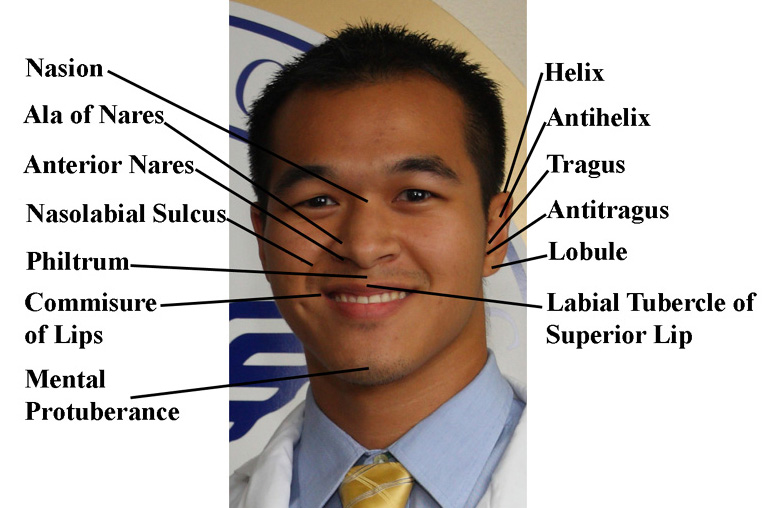
A year ago, I probably would not have been able to read the above statement, but now it’s second nature to me. Abbreviations continue to be used today by people in the medical field because it lets us write our findings faster, especially if we are pressed with time with many other patients to see. It’s also useful because it makes reading faster as well. Instead of reading “extraocular movements intact,” we could simply and briefly glance at EOMI and know exactly what it means. Ironically, however, over time the abbreviation itself becomes more intuitive to me than what it actually stands for. When I see “PERRLA” now, I instantly know what it means. But when you ask me what it actually stands for letter-by-letter, I’d have to pause for a few seconds to think about it.
While medical abbreviations has its advantages, it also has its disadvantages such as misinterpretation, especially when doctors write with their cursive Chinese calligraphic handwriting that they are so famous for. U’s can be confused with 0’s. IU’s can be confused with IV’s. Because of this, many hospital have discouraged the use of certain abbreviations like QD, QOD, U, IU, MS, and MgSO4, and have a set of approved abbreviations for current use.
Medicine really is a world of its own, with its own culture, knowledge, system, laws, traditions, ethics, practices, and of course, language. The longer we are immersed in it, the more we find ourselves expressing ourselves through it. I’ve heard residents talk like this before: “They’re showing the movie q3 hours. We should go ahead and buy tickets times 2 for the next showing.” I haven’t gotten to that level yet, but perhaps one day I may and not even realize it.
Translation:
The patient is an 80-year old white female with a past medical history of non-insulin dependent diabetes mellitus for 10 years and hypertension who complains of headache. She denies nausea, vomiting, chest pain, shortness of breath, or abdominal pain. Physical exam shows that she is alert and oriented to person, time, and place. She is not in acute distress. Her pupils are equal, round, and reactive to light and accomodation, and extraocular movements are intact. She has moist, mucous membranes, and has no jugular venous distension. Her S1 S2 sounds are present and her heart has regular rate and rhythm. Her lungs are clear to auscultation, her abdomen is non-tender and non-distended, and her bilateral pedal pulses are present. Her vital signs show a temperature of 98.3 degrees, blood pressure of 150/80, pulse of 80, and respiratory rate of 18.












Hi Benji, thanks for all your posts. My son is 4 weeks away from completing first semester, and proud to say that his scores have been very good. Spoke to him today (Thanksgiving day) and all is well, but this is the first time he commented about how tired he is. I know it was quite some time ago, but do you remember back to first semester and your fatigue level? Were you able to recharge over the 2 or 3 week Christmas break?
Thanks again,
Bill
Hi Bill,
Great to hear your son is doing well. First semester is definitely challenging as one adjusts to a strenuous medical curriculum. It just makes the winter break feel so much more relaxing and wonderful. I’m sure your son will have a great 2-3 weeks at home. Its long enough to get the rest one needs but not too long to forget everything we learned from the semester before.
Best of luck to your son,
Benji
Every time I speak to you, I get PVCs. I’m so glad I get to talk to you at least BID, otherwise I may get SOB and start drinking to the point where I have to ask myself CAGE. Can’t wait to see you soon!
Good one Irone! Can’t wait to see you ASAP!