Empiric Antibiotic Therapy for Pneumonia
How Do We Get Pneumonia?
Our body has a pretty good natural barrier to protect the lungs from potential pathogens. First, we have hair and turbinates in our nose to block out larger particles. Then we have cilia that constantly sweep mucus-trapped pathogens out of our bronchioles and trachea, and not to mention a cough reflex. We also have tons of “good bacteria” in our mouths and pharynx that crowds out the “bad bacteria” and prevents it from sticking to us. In the alveoli, we have macrophages that get rid of the pathogens that make it to the depths of the lungs, but if the macrophages become saturated with pathogens, then the alveoli can become infected. Pneumonia happens when pathogens, whether in the normal flora or exogenous, get past all the body’s natural barriers and defenses (i.e. via aspiration), and infects the alveoli of the lungs. The body reacts to the pathogens, causing inflammation, leading to coughing, sputum, and high fever.
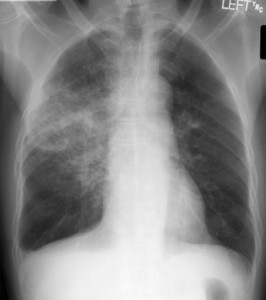
Diagnosis of Pneumonia
Whenever you suspect pneumonia in a patient after physical examination, the best way to make a diagnosis is by a chest x-ray. Seeing lobar congestion on the x-ray will tell you that you have pneumonia, but will not tell you what bug caused it. In order to do that, you will need a sputum or blood culture, which has variable accuracy. However, since sputum culture takes several days to come back with results, it’s best to go ahead and start treating the patient so that they don’t have to suffer and risk getting worse. Also, in most outpatient and inpatient settings, it’s also usually not that important to know exactly what organism is causing the pneumonia because the empiric treatment is almost always successful in treating the pneumonia. Only in the most severe cases, like when empiric therapy is not working, should blood and sputum culture to detect the exact organism be recommended.
A method commonly used to determine the severity of the pneumonia is CURB-65, which stands for:
- Confusion
- Uremia (BUN > 20mg/dL),
- Respiratory rate of over 30 breaths/minute,
- Blood pressure (systolic < 90 mmHg or diastolic < 60 mmHg)
- 65 yrs old or older.
- Score of 0-1 means outpatient treatment is indicated
- Score of 2 means hospital admission is indicated.
- Score of 3 or higher means the patient should be admitted to ICU.
- Score of 0 — 0.7% mortality
- Score of 1 — 2.1% mortality
- Score of 2 — 9.2% mortality
- Score of 3 — 14.5% mortality
- Score of 4 — 40% mortality
- Score of 5 — 57% mortality
Types of Pneumonia
In broad terms, there are two main types of pneumonia: community-acquired pneumonia (CAP) and healthcare-acquired pneumonia (HAP). Pneumonia that is acquired in the community is most likely caused by streptococcus pneumoniae, which is spread through respiratory droplets and also flourishes in most people as part of our normal flora. In most cases, we don’t know how streptococcus ends up infecting the alveoli but it does. CAP may also be caused by other organisms like gram negative (i.e. klebsiella, e. coli, morganella) or atypical bacteria (i.e. mycoplasma).
Community-Acquired Pneumonia Empirical Treatment
If a patient presents with community-acquired pneumonia without having comorbidities (i.e. diabetes, renal problems, antibiotic usage in the past few months, etc.) then the current North American standard of empiric treatment is to prescribe a macrolide, which covers gram positive, gram negative, and atypical bacteria (treatment of choice for atypicals). Of the macrolides, azithromycin or clarithromycin are preferred. Telithromycin and erythromycin are not preferred because of their adverse effects (i.e. GI effects). Erythromycin is also a hassle to take because you need to take it three times a day. Macrolide-resistant strep pneumo does exist, but it is not as important to community-acquired pneumonia patients without morbidities, so macrolides are still preferred. If the patient had used macrolides in the past 3 months before, then it’s likely that the strep-pneumo is macrolide-resistant, and therefore prescribe doxycycline instead, which also covers gram positive, gram negative, and atypical bacteria.
If comorbidities exist, then on top of macrolides, also prescribe a beta-lactam (i.e. amoxicillin, amox/clavulanate, ceftriaxone). You can also prescribe a respiratory quinolones, which are levofloxacin, moxifloxacin, gatifloxacin, or gemifloxacin. These are called “respiratory” because they are especially good at treating strep pneumo, while maintaining its efficacy on hemophilus influenza, atypical bugs, and other organisms. They also treat macrolide-resistant or beta-lactam-resistant strep pneumo, and therefore can be used alone as monotherapy in the treatment of community-acquired pneumonia with comorbidities.
Hospital-Acquired Pneumonia Empirical Treatment
Hospital-acquired pneumonia is pneumonia caught by the patient from the hospital, often when they came in for something else. They are more likely caused by gram-negative bacteria or atypicals, mainly because these pathogens are much more common in the hospital. In the non-ICU setting, the empiric treatment is the same as that for patients with CAP with comorbidities: either macrolide plus beta –lactam drugs, or respiratory fluoroquinolone monotherapy. In the Hospital ICU setting, macrolide/betalactam combo can be used, but the fluoroquinolone is recommended to also be used with betalactam as well.
So in summary, here are the empiric treatments for bacterial pneumonia:
CAP – Treat with Macrolide or Doxycycline (less indicated)
CAP with comorbidities or HAP – Treat with Macrolide + Beta-lactam, or Respiratory quinolone monotherapy
HAP ICU – Treat with Macrolide + Beta-lactam, or Respiratory quinolone + Beta-lactamPreferred Macrolides = Azithromycin, Clarithromycin.
Preferred Beta-lactams = Amoxicillin, Amoxicillin/Clavulanate, Ceftriaxone, etc.
Respiratory quinolone = Levofloxacin, Moxifloxacin, Gatifloxacin, Gemifloxacin.If you suspect MRSA involvement, add linezolid or vancomycin
If you suspect Pseudomonas involvement, use an antipseudomonal beta-lactam drug like piperacillin/tazobactam, cefepime, imipenem, or meropenem.If you are allergic to beta-lactams, substitute it with aztreonam.
My references: Up-to-Date, MedScape, Harrison’s Principles of Internal Medicine









