Seizures You Might See in Children
When you first see a seizure, or experience it yourself for the first time, it can be quite freightening. Seizures can present in numerous different ways, often not what we think of when we usually think of “seizures.” Here, I’d like to present a few types of seizures and epileptic syndromes you may see in children.
First, a little about seizures and epilepsy:
- Seizure refers to the episode of electrical discharge in the brain, whereas epilepsy refers to the disease in which recurring seizures occur.
- There are two main categories of seizures: Partial and Generalized.
- Partial (focal) seizures involve only part of the brain. It can present in different ways depending on where in the brain the seizure is occurring. If it occurs in the motor cortex, you may get uncontrolled muscle jerks for a few seconds to minutes. If it occurs in the occipital lobe, you may see flashy lights or visual hallucinations. If in the temporal lobe, where most partial seizures take place, you may get confusion, deja vu feelings, jaime vu feelings, dizziness, temporary memory loss, etc. These are all called auras. Partial seizures are divided into two types:
- Simple Partial seizures — consciousness, memory, or awareness is maintained.
- Complex Partial seizures — consciousness, memory, or awareness not maintained. Need MRI to rule out abnormalities in temporal lobe. Rx with Carbamazepine.
- Generalized seizures involve the entire brain, and can be divided into:
- Absence seizures (petit mal) — short duration, looks like blank stare, and sometimes some eye flickering.
- Myoclonic seizures — a short muscle jerk that lasts less than 1 second. They may happen together as a cluster.
- Tonic seizure — when your muscle suddenly stiffens up without letting go for several seconds.
- Clonic seizures — when your muscles does repetitive jerking movements for several seconds or minutes.
- Tonic-clonic seizures (grand mal)– when you have a sudden stiffening of muscles for a few seconds (tonic seizure) followed by repetitive muscle jerking afterwards (clonic seizure). This is what most people think of when they think of “seizures.”
- Atonic seizures — when you lose muscle tone briefly.
- Partial (focal) seizures involve only part of the brain. It can present in different ways depending on where in the brain the seizure is occurring. If it occurs in the motor cortex, you may get uncontrolled muscle jerks for a few seconds to minutes. If it occurs in the occipital lobe, you may see flashy lights or visual hallucinations. If in the temporal lobe, where most partial seizures take place, you may get confusion, deja vu feelings, jaime vu feelings, dizziness, temporary memory loss, etc. These are all called auras. Partial seizures are divided into two types:
- The term “ictal” refers to seizures. Pre-ictal describes the state before seizures, and post-ictal describes the state after seizures. Inter-ictal describes the state between seizures.
Febrile Seizures
Some kids who are genetically susceptible to febrile seizures may develop generalized seizures when they get fevers. The onset of seizures is not dependent on high the temperature goes, but rather on how quickly the temperature goes up. Having a higher temperature doesn’t necessarily correlate to a greater risk in developing the seizures. It usually happens in kids 6 months to 5 years old. There are two types. Simple Febrile Seizures are the most common, last less than 15 minutes, are generally harmless, does not recur in 24 hrs, and usually involve the entire body. The only treatment is to alleviate the fever. Antiepileptic medications are contraindicated because the adverse effects of these drugs are more dangerous than the epilepsy that they treat. On the other hand, it is Complex Febrile Seizures if it last more than 15 minutes, reoccur in 24 hrs, or is focused rather than generalized. Treatment may be considered, but must be individualized to the patient’s risks.
Childhood Absence Epilepsy
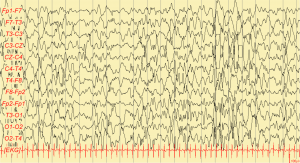
Childhood Absence Epilepsy is characterized by recurrent absence seizures (petit mal seizures, which remember is generalized). The cause is genetic and the seizures are brief and usually last less than 20 seconds. Unlike other seizures, there are no convulsions and affected kids present with a sudden-onset blank stare into space. The child may be playing or talking when it happens, and resume playing or talking immediately after the seizure without being aware of what had just happened (no postictal confusion). It is often mistaken as daydreaming and is important for school teachers to recognize. Most patients outgrow it by adulthood. On EEG, you will see a 3Hz spikes and slow waves, and this is used for diagnosis. Antiepileptic therapy with Valproic Acid or Ethosuxamide (which is particularly specific for Absence Seizures) is indicated. A lot of things can trigger absence seizures in a genetically-susceptible child, particularly stress and hyperventilation, and diagnosis can be made by telling a child to over-breathe for a few minutes to induce the seizure.
Juvenile Myoclonic Epilepsy
Juvenile Myoclonic Epilepsy (JME) is another common epileptic syndrome that usually first appears during adolescence, and persists through adulthood. It is genetic and idiopathic, not caused by tumor, trauma, or encephalitis. You experience myoclonic jerks in the mornings, typically right after you wake up (remember myoclonic seizures are generalized muscle jerks that usually last less than 1 second). In addition, most patients with JME also develop tonic-clonic seizures or absence seizures although not as often as the myotonic jerks. The seizures can be triggered by many things including light, stress, alcohol, or lack of sleep. A typical scenario would be a college student who stays up late studying (or drinking) and the next morning experiences a lot of muscle jerks, which may or may not be followed by a tonic clonic seizure. While patient history is usually enough to make the diagnosis, EEG is the most accurate. You’ll see 4-6 Hz polyspike and slow waves on EEG. Treatment is with antiepileptic drugs, particularly valproic acid. Despite the need for lifelong treatment, JME has good prognosis.
Infantile Spasms
These can happen in infants 4-8 months old and present as symmetric spasms of the trunk, neck, and extremities. They look like moro reflexes (except not triggered by stimulus), and they happen numerous times a day, sometimes even hundreds of times in a day. On EEG, you’ll see hypsarrhythmia (“high” or “lofty” waves). They are often caused by a damaged brain and can be seen in West Syndrome and Tuberous Sclerosis, and therefore you often see developmental delays or mental retardation in infants with infantile spasms. These babies often have increased corticotropin releasing hormone (CRH), leading to increased neuronal excitability, causing the spasms. The treatment is ACTH, which suppresses CRH production. Prognosis is really poor, and most patients do not survive past 10.
My Sources: MedScape, UpToDate, YouTube, Kaplan, my attending physician









