When to Think About Temporal Arteritis
When an older patient comes in for a headache, besides the common headaches like migraine, cluster, and tension headaches, it is also very important to consider Temporal Arteritis. Here, I will explain to you what this is.
What is it?
In summary, temporal arteritis, also known as Giant Cell Arteritis, is a systemic vasculitis of medium and large arteries.
While the exact cause is still unclear, there is evidence that temporal arteritis has both environmental and genetic causes. People with a specific gene variation on HLA-DR4, A31, B40, or Cw3 who are then exposed to certain viruses and bacteria are more likely to get an inflammatory reaction to their medium and large-sized arteries. This in turn can cause abnormal narrowing of these arteries, decreasing the blood supply to organs that are supplied by these arteries, as well as blood clots within these arteries. Furthermore, this may cause you to also experience fever, weight loss, anemia, and fatigue.
While temporal arteritis can potentially occur in any medium to large-sized artery, it most often occur in temporal, external carotid, vertebral, and ophthalmic arteries. Because these arteries are all on the face and head, it can give you facial pain and headache, particularly feeling a throbbing pain on the side and back of the head. Inflammation of the maxillary artery can decrease the blood supply to the muscles of the jaw, causing jaw pain when chewing. Inflammation of the ophthalmic artery supplying the eyes can cause vision problems, particularly sudden-onset irreversible blindness, which is the most important thing you have to worry about when someone has temporal arteritis, because you can’t reverse it. Because inflammed arteries can cause narrowing of the arteries, blood can collect there and form clots. If these clots dislodge from the arteries, they can travel to the brain and cause strokes. Temporal arteritis is also associated with aortic aneurysm, dissection, and rupture.
What do you see on physical exam?
The temporal artery runs along the side of the face and so if you get inflammation there, you will see a thick artery running along the affected side of the head that does not have pulse. The patient will also often feel pain when you touch the scalp on the affected side.

How many people are affected?
15-25 of every 100,000 people are diagnosed with temporal arteritis every year. Most are over 50 years old and the average age of diagnosis is 71 years old. It is the most common systemic vasculitis in adults in the Western world. Women are twice more likely to get it than men, and Caucasians are more likely to get it than other ethnicities. It is not common in Blacks or Asians.
Differential Diagnosis
When you see symptoms of temporal arteritis, you should also consider and rule out possible lupus, primary systemic amyloidosis, rheumatoid arthritis, polyarteritis nodosa, takayasu arteritis, and polymyositis.
How do you diagnose temporal arteritis?
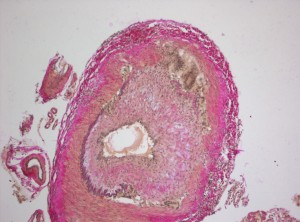
When you suspect temporal arteritis, you should run some lab tests like ESR and C-reactive protein levels, which will both increase if the patient has temporal arteritis. While these lab tests are great for initial screening, they are very non-specific and only tells you the patient has some sort of inflammation, whichever the cause may be. Therefore you should always do a temporal artery biopsy afterwards to truly diagnose the patient with temporal arteritis. You should get about 2-3 cm of biopsy and take a look at it. An artery with temporal arteritis would look thick and fibrous with a “tree bark appearance” due to fragmented internal elastic lamina, and loss of medial smooth muscle. You will also see skip-lesions, meaning there is a segmental distribution of the inflammatous infiltrates. You will also see Giant Cells, which are multinucleated macrophages that contribute to the inflammation, hence it’s other name “Giant Cell Arteritis.”
How do you treat temporal arteritis?
Corticosteroids, particularly prednisone. It’s important to treat as soon as possible to prevent irreversible blindness from happening. With treatment, most patients become symptom-free after3 years of therapy. Long-term corticosteroid use, however, has its own set of adverse effects, like cataracts, hypertension, myopathy, and osteopenia, and therefore patients often take other things to prevent these side effects as well, like Vitamin D and Calcium to build up stronger bones to prevent the osteopenia.
How do you prevent temporal arteritis?
There are no known prevention methods. Just make sure to see a doctor if you are older and have headache.











I noticed Caucasians are targets for a lot of diseases, could it be due to the diet? Could certain meat proteins contribute to these diseases? For example Osteoporosis is genetically linked to white Caucasian females over African descent females because Caucasians have lower bone mass.